Abstract
Background: In pediatrics, acquired aplastic anemia (AA) is most commonly due to infection, particularly viruses, when a cause can be identified. Coronavirus disease 2019 (COVID-19) has affected more than 197 million people worldwide, and children typically experience a less severe disease course. COVID-19 is known to cause transient hematologic abnormalities, including leukopenia, lymphopenia, anemia and thrombocytosis or thrombocytopenia in severe cases.
Objectives: Describe three cases of COVID-19 associated acquired aplastic anemia in immunocompetent pediatric patients.
Design/Methods: Case series established by retrospective review of the electronic medical record.
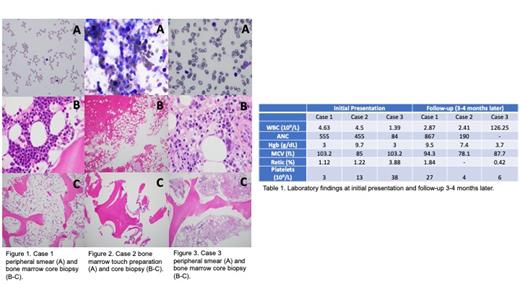
Results: Case 1: An 8-year-old Hispanic male presented with a three-week history of increased bruising and a one-week history of progressive exercise intolerance, shortness of breath, pallor and fatigue. Labs showed pancytopenia. Bone marrow aspirate and biopsy was markedly hypocellular at 5-10% consistent with aplastic anemia (Figure 1). Work-up for the etiology of his aplastic anemia was only significant for positive SARS-COV-2 antibodies and a SEC23B variant of unknown significance on a comprehensive bone marrow failure (BMF)/myelodysplastic syndrome (MDS)/leukemia panel from the Children's Hospital of Philadelphia (CHOP). He was treated with eltrombopag olamine and then proceeded to immunotherapy with cyclosporine (CsA) and horse antithymocyte globulin (ATG) when a sibling match was not identified for hematopoietic stem cell transplant (HSCT). Three months later, his peripheral blood counts have improved, and he is no longer transfusion-dependent. Repeat bone marrow aspirate and biopsy continues to show markedly hypocellularity at <5%.
Case 2: A 5-year-old non-Hispanic white female presented with a two-week history of easy bruising, petechial rash, fatigue and bone pain. Labs showed pancytopenia, and bone marrow aspirate and biopsy showed marked hypocellularity at 5-10% consistent with aplastic anemia (Figure 2). Her aplastic anemia work-up was significant for positive SARS-COV-2 antibodies and subclinical RBC and WBC paroxysmal nocturnal hemoglobinuria (PNH) clones. She was started on eltrombopag olamine and then proceeded to immunotherapy with CsA and ATG when a matched sibling donor was not identified. Three months later, she continues to be severely neutropenic, anemic and thrombocytopenic requiring multiple transfusions. Repeat bone marrow aspirate and biopsy showed variable cellularity with some areas 10-20% and others 70% with an overall cellularity of 50%.
Case 3: An 8-year-old non-Hispanic white female presented with a 10-day history of fatigue, bilateral leg pain and pallor. Labs showed pancytopenia, elevated inflammatory markers and elevated hemoglobin F. Bone marrow aspirate and biopsy demonstrated mild-moderate hypocellularity at 40-50%, left-shifted myelopoiesis and dyspoiesis in the erythroid and megakaryocytic cell lines (Figure 3). MDS and acute lymphoblastic leukemia (ALL) fluorescence in situ hybridization (FISH) panels were negative. Additional work-up revealed positive SARS-COV-2 antibodies. Her pancytopenia resolved within two weeks of her initial hospitalization. Four months later, she presented with increased bruising and fatigue. Labs showed leukocytosis, thrombocytopenia, anemia and circulating peripheral blasts. Bone marrow aspirate and biopsy was consistent with B-cell ALL. She is receiving chemotherapy on study COG AALL1732.
Conclusion: Severe aplastic anemia (SAA) has high morbidity and mortality, and timely diagnosis is needed for appropriate treatment. Multiple different viral infections have been known to cause acquired aplastic anemia. Data on all the sequelae of COVID-19 infection is still emerging, but it is plausible that COVID-19 infection may cause SAA. All three patients were found to have positive COVID-19 antibodies but did not have any evidence of previous COVID-19 infection. Further research and follow-up is needed to determine if previous COVID-19 infection is indeed a risk factor for development of SAA.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal